

Goodwin University

The Importance of Community Health Education – and Where You Might Fit In
Community health education is an important part of our world today. In fact, if the year 2020 has taught us anything, it is that community health education is a vital part of our society. The outbreak of COVID-19 – a pandemic that has infected millions of people around the world — crippled the global economy and changed the way we live. However, there have also been great strides made in preventing the spread of the novel coronavirus, thanks to infectious disease experts and public health educators who work diligently to keep the public informed.
One of the few positive outcomes of this life-changing virus has been the acts of kindness — big and small. Doctors and nurses have been working 18-hour shifts in areas hit hardest by the outbreak, and healthcare workers in other areas have flown to major cities to volunteer their services. Manufacturers have been shifting focus toward producing personal protective equipment (PPE) and donating thousands of items to hospitals. Even amateur crafters have been hard at work making cloth masks to donate to their local nurses! These powerful signs of hope may have inspired you to take action. It may even inspire you to make a career change, or help you decide what you’d like to do with your life.
One of the most important roles in public health today is in community health education. Public health educators teach people about behaviors that promote wellness. Within this field, there is a variety of public health issues to address, such as disease prevention, environmental health, nutrition, safety and disaster preparedness, and more.
Public health educators typically work in public health divisions of states, counties, cities, and towns. They may also work in private sectors, such as health insurers or counseling programs. They often create and assess health education programs, write grants and find proposals, conduct research, and oversee health education programs within their communities.
Whether working with individual residents, organizations, or entire populations, public health educators make a real impact on society. But what exactly can you do within community health education? Where do these types of health professionals fit?
There are many different paths available in the public health education field. The job opportunity for aspiring public health professionals is bright. In fact, the U.S. Bureau of Labor Statistics (BLS) expects employment of community health educators to grow 11% over the next several years.
Professionals who specialize in this field may work in the following settings:
- Community Health
- Consumer Health
- Environmental Health
- Family Life
- Mental/Emotional Health
- Injury Prevention and Safety
- Personal Health
- Prevention and Control of Disease
- Substance Use or Abuse
But how does one break into the community health education field ? According to the BLS, health educators need a bachelor’s degree before teaching others about health and wellness. Depending on the area of focus, public health educators may also need to earn the Certified Health Education Specialist (CHES) credential before starting their careers. This also requires a bachelor’s degree, and is where an undergraduate public health program comes in handy.
A Bachelor’s in Public Health , such as the one at Goodwin University, can prepare you for a future of powerful impact. Classes at Goodwin are taught by industry professionals who understand the inner workings of the public health field. Their experience can prepare you better than any textbook ever could. The program at Goodwin is also one that offers flexibility to students. Courses are available days, nights, and even in a hybrid online/on-campus format. This offers the kind of flexibility needed to complete a degree without putting your life on hold.
You may dream of working for the Centers for Disease Control and Prevention (CDC) or the World Health Organization (WHO) to help tackle massive pandemics like COVID-19. Or perhaps you have a passion for health and wellness and want to make a positive impact on your own local community. Either way, the Career Services team at Goodwin can help you get there. This group of passionate professionals is available to Goodwin students and grads — for free — for life. The Career Services team does not stop until you are in a role that you love.
Are you ready to jumpstart your career in community health education? You will make a positive impact in your community — or around the world — within no time once you have completed your degree. Learn more about the Public Health program at Goodwin University by calling 1-800-889-3282, or visit us online to request more information.

Goodwin University is a nonprofit institution of higher education and is accredited by the New England Commission of Higher Education (NECHE), formerly known as the New England Association of Schools and Colleges (NEASC). Goodwin University was founded in 1999, with the goal of serving a diverse student population with career-focused degree programs that lead to strong employment outcomes.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Education Improves Public Health and Promotes Health Equity
Robert a hahn, benedict i truman.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Robert A. Hahn, Centers for Disease Control and Prevention, 1600 Clifton Road NE, MS E-69, Atlanta, GA 30333, USA. [email protected]
Issue date 2015.
Reprints and permissions: sagepub.com/journalsPermissions.nav
This article describes a framework and empirical evidence to support the argument that educational programs and policies are crucial public health interventions. Concepts of education and health are developed and linked, and we review a wide range of empirical studies to clarify pathways of linkage and explore implications. Basic educational expertise and skills, including fundamental knowledge, reasoning ability, emotional self-regulation, and interactional abilities, are critical components of health. Moreover, education is a fundamental social determinant of health – an upstream cause of health. Programs that close gaps in educational outcomes between low-income or racial and ethnic minority populations and higher-income or majority populations are needed to promote health equity. Public health policy makers, health practitioners and educators, and departments of health and education can collaborate to implement educational programs and policies for which systematic evidence indicates clear public health benefits.
Keywords: equity, disparities, social determinant, health in all policies
Education is a process and a product . From a societal perspective, the process of education (from the Latin, ducere, “to lead,” and e, “out from,” yield education, “a leading out”) intentionally engages the receptive capacities of children and others to imbue them with knowledge, skills of reasoning, values, socio-emotional awareness and control, and social interaction, so they can grow as engaged, productive, creative, and self-governing members of a society. 1 Of course, not all educational institutions achieve these goals for all children – far from it; educational institutions in the United States often fall short of goals, and too many students may be led into school failure, social dysfunction, and marginal living conditions with lifelong disadvantages.
Not all learning is acquired in a formal school setting. The process of education occurs at home, in school, and in the child’s community. Children in the United States spend a relatively small proportion of their waking hours in school – approximately 1,000 hours per year or about one fifth of their waking hours. 2 Thus there are many opportunities for informal education outside the school setting. 3 When researchers find evidence linking mental capacities, knowledge, feelings, and values with health outcomes, 4 not all consequences can be attributed to formal education.
As the product of the educational process, an education is the array of knowledge, skills, and capacities (ie, intellectual, socio-emotional, physical, productive, and interactive) acquired by a learner through formal and experiential learning. An education is an attribute of a person. And, although a person may be said to “have” a certain level of education at any particular moment, educational attainment is a dynamic, ever-evolving array of knowledge, skills, and capacities.
Although we conceive of education broadly, including both its formal and informal sources, the focus of our evidence review is the formal education that is measured in most research. Our recommendation also focuses on the formal education, from early childhood to college and beyond, that is, the subject of educational policy and, we argue, should also be the subject of public health policy.
In public health, researchers and practitioners have examined 3 principal relationships between education and health. First, health is a prerequisite for education : hungry children or children who cannot hear well, or who have chronic toothaches, eg, are hindered in their learning. 5 Second, education about health (ie, health education) occurs within schools and in many public health interventions; it is a central tool of public health. 6 Third, physical education in schools combines education about the importance of physical activity for health with promoting such activity. 7 Here we focus on 2 additional relationships between education and health. First, we propose that education as a personal attribute is a central conceptual component and essential element of health , similar to physical fitness. Second, we summarize the extensive literature demonstrating that formal education is a contributing cause of health .
We argue that education – the product and personal attribute acquired – is both a critical component of a person’s health and a contributing cause of other elements of the person’s concurrent and future health. Consistent with other definitions of health, a person who lacks basic elements of an education is not fully healthy. 8 , 9 For example, the 1978 Alma Ata International Conference on Primary Health Care defined “health” to include “a state of complete…mental and social well-being” – which we see as largely products of education. Attainment of a certain level of formal education by young adulthood affects lifelong health through multiple pathways. 8 , 10
We then argue that, because it is both an essential component and a major contributing cause of health, educational achievement broadly should be a legitimate arena for public health intervention. Thus, public health practitioners could legitimately promote educational programs to advance public health. Education should also be recognized as an essential requirement for the disruption of the cycle of poverty and inequities in health. The public health community should expand research to better understand the causal relationships between education and health, and thereby identify evidence-based educational policies that have great potential to improve public health.
A Broad Concept of Education
We propose a broad concept of education as a personal attribute, which includes not only subject-matter knowledge, reasoning, and problem-solving skills, but also awareness of one’s own emotions and those of others and control of one’s emotions (ie, “emotional intelligence”) 11 and associated abilities to interact effectively. “Education improves health because it increases effective agency, enhancing a sense of personal control that encourages and enables a healthy lifestyle. Education’s beneficial effects are pervasive, cumulative, and self-amplifying, growing across the life course.” 12
In 1983, the National Commission on Excellence in Education’s report, A Nation at Risk , launched a national conversation about the need for educational reform. 13 In 1990, the US Department of Labor initiated a program – the Secretary’s Commission on Achieving Necessary Skills – to determine critical capacities for a US workforce to be provided by the educational system. 14 The capacities proposed were based on “a three-part foundation” reflecting the broad notion of education that we propose: Basic Skills (reading, writing, arithmetic, mathematics, listening, speaking), Thinking Skills (creative thinking, decision making, problem solving, seeing things in the mind’s eye, knowing how to learn, reasoning), and Personal Qualities (responsibility, self-esteem, sociability, self-management, integrity/honesty). The project recommends as a central educational goal: “All American high school students must develop a new set of competencies and foundation skills if they are to enjoy a productive, full, and satisfying life.” 14 (p1) We would expand this list of outcomes to include a healthy life.
Education as an Element of Health
In our conception, basic education is an integral part of being healthy. A person is unhealthy if he or she lacks basic knowledge, the ability to reason, emotional capacities of self-awareness and emotional regulation, and skills of social interaction. These embodied personal attributes or mental capacities, the products of formal education as well as other learning experiences, are conceptually comparable to physical capacities of fitness and coordination – well-established components of health. “Education teaches a person to use his or her mind: Learning, thinking, reasoning, solving problems, and so on are mental exercises that may keep the central nervous system in shape the same way that physical exercise keeps the body in shape.” 8 (p738) A person is unhealthy who cannot conduct himself or herself effectively and achieve some level of “social well-being” – a critical element of the World Health Organization (WHO) conception of health, which recognized the contributions of social sectors beyond the health sector in promoting health. 9
The projects of several US and international health agencies reflect this concept of education as a component of health. For example, the US Centers for Disease Control and Prevention recognizes “cognitive health” in its Healthy Aging Program; although the focus of this program is prevention and control of Alzheimer’s disease, the “cognitive health” rubric suggests far broader considerations: “The public health community should embrace cognitive health as a priority, invest in its promotion, and enhance our ability to move scientific discoveries rapidly into public health practice.” 15 (p1) The National Institutes for Health similarly has a “healthy brain” program that recognizes cognitive as well as emotional capacities as elements of health. 16
Similar concepts are recognized internationally by the WHO, in accordance with its definition of health cited above. More recently, a WHO paper 17 included cognition and affect as 2 of 6 domains for the international comparison of health status .
Measures of Education as a Personal Attribute
Education is measured in a variety of ways. A common measure, years of schooling/educational attainment, is problematic insofar as time spent in school gives little indication of how the time is spent and what is learned. 2 School-level completion may be a better measure, but also varies in terms of the quality and quantity of what is learned. Standardized tests of subject-matter knowledge and reasoning skills may be still better for some purposes, but may offer challenges when compared across populations. 18
Some 19 , 20 have argued that teacher-assigned grades are an alternate, if not better, predictor of long-term outcomes than standardized tests because they reflect not only academic achievement, but also classroom social and learning skills that indicate abilities to learn and to interact successfully. The breadth of skills addressed by this measure better reflects the broad concept of education argued here. Subjectivity, personal preferences, and comparability are challenges with teacher-assigned grades as a measure of achievement.
Evidence of Causal Association
It may seem odd that, in the perspective developed here, education – the product and the personal attribute – is at once an element of health and a cause of health. The relationship is similar to that of physical fitness and health. Fitness is an element of health and an important cause of subsequent health – not only of physical fitness, but of other facets of health as well, including cardiac health and mental health. 21 – 23 In addition to providing extensive evidence that education is associated with health, we argue that the underlying causal process is conceptually similar to the causal relationships between physical activity or an infectious agent and health. We provide some evidence of causation, noting that the notion of causal proof in a traditional deterministic sense has been challenged. 24
Criteria to determine causality in public health developed by Sir Bradford-Hill in 1965 25 are still useful. They are:
Strength of association linking hypothetical cause and outcome (as assessed, eg, by the magnitude of relative risks)
Consistency of findings, eg, by different researchers in different settings
Specificity – the connection of specific, narrow causes to specific outcomes
Temporal sequence—the necessity of cause preceding consequence
Dose–response relationship
Plausibility in terms of current knowledge
Coherence – similar to plausibility, the fit with other contemporary knowledge
Experiment – offering the strongest support
Analogy – the comparability of postulated causality with causality in similar phenomena
Most of the Bradford-Hill criteria clearly apply when linking education to health. An obvious exception is specificity, because education itself is a broad concept including many elements, and the causal consequences of education are also numerous and heterogeneous. Bradford-Hill did not regard specificity as essential, as in the case of cigarette smoke with its multiple health consequences. As Susser has argued, “Specificity enhances the plausibility of causal inference, but lack of specificity does not negate it.” 26 (p153)
The associations presented below satisfy several standard criteria for causation. At least 3 approaches are used: 1) observational cohort studies with concurrent controls, 2) natural quasi-experiments in education policy, and 3) educational experiments. In the sections that follow, we provide samples of evidence of the causal association between education and health, assessed first by various health-related outcomes: health risk and protective behaviors, wages and income (resources for health), self-assessed health, morbidity, mortality, and life expectancy. We then provide evidence from experimental studies. The literature on these topics is extensive 4 , 8 and here we describe only a few examples, from early childhood and beyond. Evidence of the association between measures of education – the personal attribute – and other health-related outcomes is positive, strong, and consistent.
Health Risk and Protective Behaviors Are Associated With Academic Achievement
Evidence of an association between high school student grades and risk behaviors in the United States is remarkably consistent; higher average grade achievement is associated with lower rates of risk behavior ( Figure 1 ). 27 One plausible explanation is that there is causation in the reverse direction of what is proposed here, ie, that risk behavior interferes with academic achievement; such reverse causation seems reasonable, eg, for watching television and using alcohol. Also plausible is that other factors, such as strong values, promote both academic achievement and self-protective behaviors, or that academic achievement is associated with knowledge, which leads to risk avoidance. Another explanation is that underlying psychological or environmental conditions are associated with risk behavior and academic problems. Causation in both directions is likely. The consistency of a dose response for multiple behaviors is consistent with an effect of educational success on the avoidance of risky behavior.
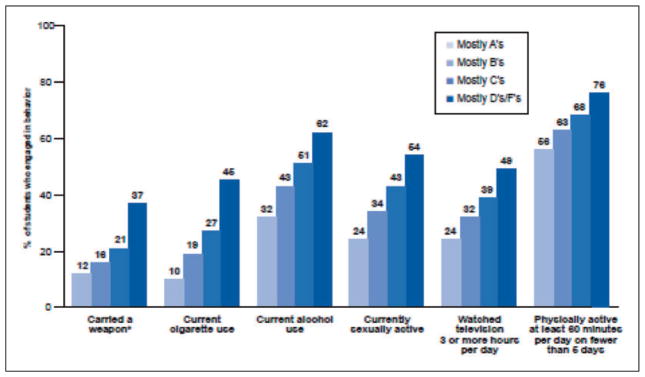
Health-risk behaviors and school grades, United States, 2009.
Source: www.cdc.gov/healthyyouth/health_and_academics/pdf/health_risk_behaviors.pdf .
There is also strong evidence of a dose response between years of education and many health-related risk and protective behaviors among US adults. Analysis of a representative survey of adults aged >25 years between 1990 and 2000 indicates that the prevalence of several risk behaviors is generally higher among those with fewer than nine years of formal education, begins to decline among those who have nine to 12 years of formal education, and continues to decline with additional years of education; this finding corresponds to the recognized importance of high school completion for subsequent health. 28 , 29
Wages and Income, Resources for Health, Are Associated With Educational Success
Wages and income are not health outcomes, but are closely linked with health outcomes because they provide access to health-related resources, such as healthy food, a safe environment, and healthcare. A recent analysis 30 of trends in US wages over more than 20 years finds higher wages consistently associated with higher educational attainment and a trend toward increasing differences in wages by educational status. In the causal chain, high educational attainment is antecedent to high wages or income. A recent study 31 linking individual kindergarten standardized achievement tests with wages at ages 25–27 years indicates a remarkable linear association accounting for 17% of the variability in the wage outcome – 20 years later ( Figure 2 ). Although high family income precedes and predicts educational success in children, controlling for such demographic characteristics of the kindergartner (including family income, household ownership, and marital status) diminishes, but by no means eliminates, the association found in this study.
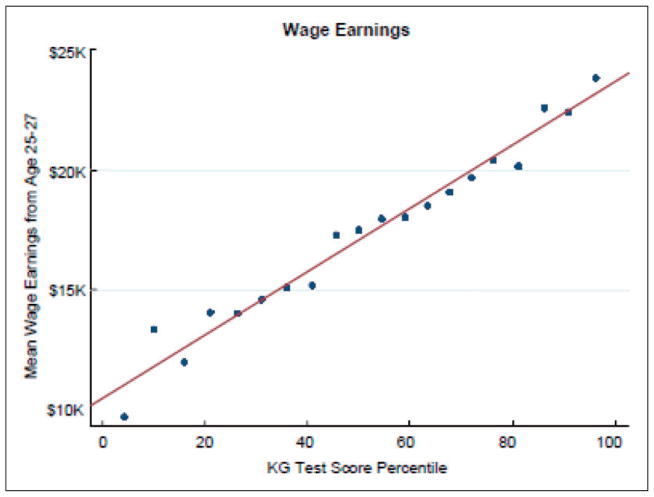
Association between kindergarten test score percentiles and mean wage earnings, ages 25–27 years, Tennessee STAR program.
Source: Chetty, 2010.
Self-Assessed Health Is Associated With Educational Attainment
Self-assessed health is a well-established index of morbidity and predictor of mortality. 32 , 33 A recent study compares the association of educational attainment with self-assessed health in US and Canadian populations. 34 , 35 Controlling for basic demographics and income, those with less than a high school education in the United States are 2.4 times as likely as high school graduates and 4.1 times as likely as those with post-secondary education to rate their health as poor. Further adjusting these ratios for risk behaviors only moderately reduces the ratios, suggesting that education is related to self-reported health due to important factors in addition to risk behaviors.
It is plausible that health status affects the likelihood of educational achievement, but it is likely that the major force of causation is in the opposite direction. Not only is educational attainment closely associated with self-rated health, but the association increases with age when measured by the number of days per week reported as free of major symptoms. With increasing age, the gap in symptom-free days increases between those with a college degree, those with a high school degree or some college, and those with less than a high school degree, suggesting that the effects of education are pervasive throughout the lifespan, and that its consequences have cumulative effects on health over time. 36
Morbidity is Associated With Educational Attainment
In the United States, although higher self-reported rates of several conditions, such as prostate cancer and sinusitis, are reported among more adults with greater levels of education, for most conditions the reverse direction of association is evident. Rates of major circulatory diseases, diabetes, liver disease, and several psychological symptoms (sadness, hopelessness, and worthlessness) show higher rates among adults with lower educational attainment. 35
Mortality and Life Expectancy Are Associated With Educational Attainment
Evidence also exists of a strong association between educational attainment and mortality from many diseases. 37 The parallel relationship for three heterogeneous groups of illness or injury again suggests an underlying connection unrelated to the specific etiologic pathways of each cause of death ( Figure 3 ). 37 In addition, the modal age for completing formal education (the mid-20 s) substantially precedes the peak age for mortality in the United States (77 years of age) by many years, consistent with another Bradford-Hill principle, ie, the precedence of cause before effect.
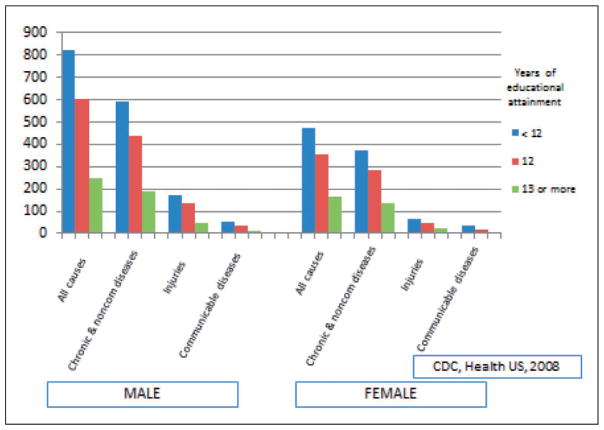
Age-adjusted death rates among persons ages 25–64 years for several condition groupings, by sex and educational attainment. Selected US states, 1994–2005.
From the perspective of life expectancy, at age 25 in 2005, a man in the United States with less than a high school education could expect to live an additional 44.2 years to age 69.2 years; a man with a graduate degree could expect to live more than 15 years longer. At age 25 years, a woman in the United States with less than a high school education could expect to live to age 74.9 years; a woman with a graduate degree could expect to live more than 11 years longer. 38
Educational Experiments and Quasi-Experiments
True experiments in the field of education are uncommon. Nevertheless, several experiments have been conducted. Groups of children, often from low-income or minority families, have been exposed, sometimes with random assignment, to different forms of education and followed over time to determine long-term outcomes, including health-related outcomes, as shown in the following 3 examples of early childhood programs.
In the early 1960s, 3- and 4-year-olds with low IQs from low-income families were randomly assigned to either the High/Scope Perry Preschool Program – an educational program including home visits – or no intervention. Home visits were designed to strengthen parental engagement in the child’s education. Participants were periodically assessed until age 40. 39 Over several follow-up assessments, intervention participants had greater levels of educational attainment, income, and health insurance, lived in safer family environments, and had lower rates of tobacco and drug use and risky driving behavior than controls. At age 40 years, however, more intervention than control participants had chronic diseases, but fewer intervention participants had died.
In 1972, healthy infants at risk of academic difficulties because of their demographic circumstances (eg, poor, minority, single parents) were randomly assigned to the Carolina Abecedarian Project or a control intervention (offered social services, nutritional supplements, and healthcare services, but no educational program). 40 The Abecedarian preschool program focused on developing cognitive, social, language, and motor skills from birth through age 5 years. Before entering kindergarten, control and experimental children were again randomized into either routine schooling or a strengthened school program complemented by home visits for parental guidance to reinforce child learning. At follow-up, both the preschool and the early schooling programs were shown to be beneficial in terms of academic achievement; the preschool program had the larger effect. By age 21 years, participants in the early childhood education intervention (combining those with and without the strengthened primary school programming) had better health behaviors and better health than those who did not receive the early childhood education intervention. 41 By their mid-30 s, those exposed to the intervention, particularly males, had substantially more favorable cardiovascular risk profiles than those exposed to the control condition. 42
Finally, though not a true experiment, the Chicago Child-Parent Center program followed two groups of poor Chicago children aged 3 and 4 years: one exposed to an early childhood program and the other not exposed. Children residing in Chicago districts with federally funded kindergarten programs were eligible and selected on a “most-in-need basis”; comparison children lived in similarly poor neighborhoods with locally funded kindergarten programs. The Chicago Child-Parent Center provided educational enrichment from prekindergarten through the third grade, required parental involvement in the classroom a half-day per week, and provided nutrition and health services. At age 24 years, in comparison with control subjects, participants had lower rates of out-of-home placement (indicating child abuse), lower rates of arrests and conviction for violent behaviors, and lower rates of disability. 43
A recent review of the effects of early childhood educational programs indicates that programs with strong instructional components and those evaluated with strong study designs have large and enduring effects on the educational, social, and health outcomes of participants. 44
Several researchers have made use of natural quasi-experiments involving education policies that rapidly change years of schooling required, to evaluate the effects of the requirement on health-related and other outcomes. When state educational requirements change from 1 year to the next from 7 to 9 years, eg, cohorts of children of a certain age in that state will receive approximately 7 years of education, while their younger siblings will receive 9 years. The state where this policy is implemented may be compared by regression discontinuity analysis from before to after the change, but also with other states that have not made this change at the same time.
In one such study, Lleras-Muney 45 uses a sample of US census data to estimate the effects on mortality of changes in compulsory education requirements in 30 states, comparing birth cohorts before and after such changes between 1915 and 1939 with long-term follow-up data. Lleras-Muney concludes that each year of additional required schooling resulted in a reduction of mortality by 3.6% over 10 years, or gain of 1.7 years to life expectancy at 35 years of age. Although these data are old, it is likely that the general effects of increased educational requirements on mortality have not changed substantially. Other researchers have used regression discontinuity analysis to estimate the effects of education on rates of crime, arrest, and incarceration in the United States 46 and on teenage births in the United States and Norway. 47 Among researchers using this design, only Arendt 48 finds equivocal evidence regarding the effects of additional years of education on self-rated health, body mass index, and smoking in the United States, Canada, and Denmark. The heterogeneity of conditions affected by educational exposure again suggests a broad, nonspecific underlying “mechanism.”
The Fallacy of the Endowment Hypothesis
Gottfredson has proposed that intelligence – innate intellectual and associated ability – rather than educational attainment is the “fundamental cause” of socioeconomic inequalities in health, a proposal referred to as the “endowment hypothesis.” 49 Several basic features distinguish Gottfredson’s notion of intelligence from the concept of education as defined in this article: intelligence is regarded as “natural, not cultural,” “context-free,” and “highly heritable” – indicating a largely innate, biological foundation, little affected by environmental variability. From this vantage, education as conceived in this article may be regarded as largely determined by intelligence insofar as those with greater intelligence are both more likely to seek education and to succeed in acquiring it.
Gottfredson’s hypothesis is explicitly evaluated by others in a study of 2 US cohorts that assesses the contributions of education, income, and intelligence to 3 health outcomes: mortality, life-threatening illness, and self-rated health. 50 The researchers posit an alternative model, in which there are underlying “background influences on [socioeconomic status] and intelligence.” In this model, intelligence affects education and income, and both of these socioeconomic status characteristics in turn affect intelligence; a summary of research on this linkage 51 indicates that a year of education is associated with a gain of between 2 and 4 IQ points. In both study cohorts, intelligence during high school is measured by standardized and validated tests, the Henmon-Nelson test and the Wechsler Adult Intelligence Scale. The researchers find generally consistent evidence of pairwise dose–response associations between levels of education, income, and intelligence with each of 3 health outcomes.
The researchers then examine the questions: what is the effect of controlling the association of education and health outcomes for intelligence; of income and health outcomes controlling for intelligence; and of intelligence and health outcomes controlling for both education and income? This assessment allows answering 2 basic questions: how much does intelligence contribute to the effects of education and of income on health, ie, what are the effects of these determinants net the contribution of intelligence? And, to what extent are the effects of intelligence on health mediated by income and education? The researchers find that separately controlling the effects of education and income on health outcomes for intelligence alters the coefficients for education and income minimally and leaves all associations statistically significant at the 0.05 level or less, indicating that little of the effect of education on health is mediated by intelligence.
The effects of controlling the effects of intelligence on health for education and income are more complex. Only 1 of the 2 surveys finds a significant effect of intelligence on mortality ( P <.05); controlling for education and income eliminates the significance of this finding. Thus, the effect of intelligence on mortality is largely mediated by income and education. Both surveys find statistically significant effects of intelligence for both life-threatening illnesses and self-rated health; however, the effect magnitudes are diminished by a mean of 69.4% and statistical significance is again eliminated for all findings except for self-rated health in one of the surveys. These findings indicate that the effects of intelligence on health outcomes are largely mediated by education and income. 50 There is thus substantial evidence that education has a strong effect on health, independent of background intelligence. Innate intelligence may be a “fundamental cause” principally insofar as it leads to higher education and income.
Causal Pathways and Evidence Linking Education and Health
Building on the work of others, 10 , 52 we constructed a model indicating the three major pathways linking education and health outcomes in adulthood and including the several facets of education – knowledge, problem solving, emotional awareness and self-regulation, values, and interactional skills ( Figure 4 ). First is the psycho-social environment, including the individual’s sense of control, social standing, and social support, which reflects and bolsters capacity and agency. Second is work, through which the individual may achieve satisfaction and income, which allows access to many health-related resources. Finally, healthy behavior may protect an individual against health risks and facilitate negotiation of the healthcare system.
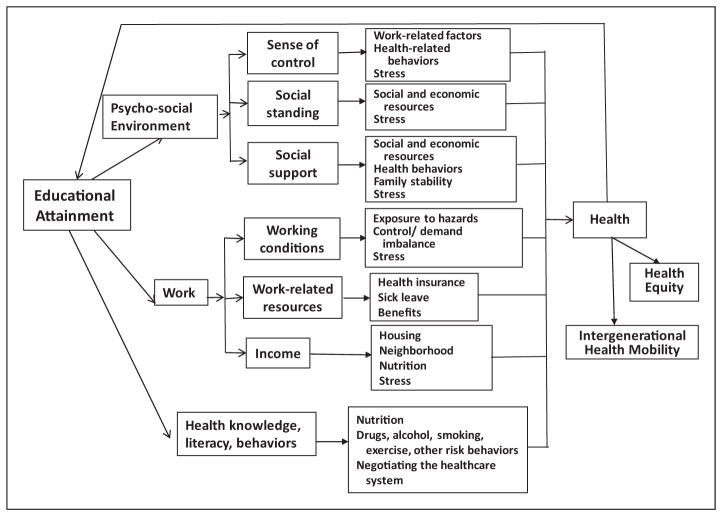
Pathways from educational attainment to health outcomes.
Ross and Wu 8 used 2 national probability samples of US adults to assess the effects of completed education on self-perceived health and reported physical functioning. They first assessed the association between education and each of three broad covariate groups – psycho-social environment; work; and health knowledge, literacy, and behaviors – that are themselves determinants of health outcomes ( Figure 4 ). 8 For each data source, they began with a model including as covariates only demographic characteristics of their samples. To the basic model, they first added employment and economic covariates, then social-psychological covariates, and finally risk behavior covariates, noting the changes in regression coefficients for educational exposures on health outcomes. This approach allowed assessment of the magnitude of each of these groups of covariates as pathways linking education to health-related outcomes. However, the relative contribution of each group of factors cannot be determined precisely, because these groups are unlikely to be causally independent, and covariate groups entered into the regression early are thus likely to show greater reductions in regression coefficients than those entered later.
In both samples, education was associated with all covariates in expected directions. The largest effect was for work-related variables, including income. Those with lower income not only had limited resources useful in maintaining health, but also may have experienced anxieties that exacerbate health problems. The effects of psycho-social resources were also statistically significant and of similar magnitude. Risk behavior and knowledge also contributed to the association between education and health by both measures. The 3 clusters of covariates together explain between 55% and 59% of the variance in self-reported health and between 46% and 71% of physical functioning in these surveys. This suggests that the smallest contribution to health outcomes is associated with health behaviors, which were entered last into the regression model. In both samples, education has a significant residual “direct” effect, independent of the three examined pathways. In summary, education’s association with improved health is attributable to greater work opportunities and rewards, a greater sense of control and social support, healthier behaviors, and a direct effect on health. Similar results are found by Cutler and Lleras-Muney, 28 who use different sources to assess associations between educational attainment, health behaviors, and mortality in the United States and Great Britain.
In a separate study, Ross and Mirowsky 53 provide evidence that the effect of higher levels of education on health is mediated principally by its contents, including values and skills imparted, and far less by means of status markers such as the diploma or the prestige of the degree-granting institution. Evidence for this conclusion derives from a regression analysis of national data including measures of years of education, receipt of diplomas, and school selectivity (based on test scores of entering freshmen). In another study, Reynolds and Ross 54 provide evidence that “the direct effect of education on well-being is greater than the direct effect of social origins, and the total effect of social origins is mediated mostly by education.” 54 (p226) Evidence derives from a regression analysis of two national data sources in which the researchers control for parental education, father’s occupation, and childhood poverty. They also find that a person’s level of education has a far greater effect on health if his or her parents were poorly educated than if they were well-educated. Unfortunately, in our society, parental and child educational levels are highly positively correlated, so that the children of parents with little education, who might benefit the most from higher levels of education, are least likely to receive that education. 55
Ross and Mirowsky 55 (pp597,598) conclude (emphasis added): “…certain policy implications follow. First, education policy is health policy. Second, health policy must address the educational opportunities of children raised by poorly-educated parents. Otherwise those children, in adulthood, will suffer the multiplicative health consequences of low parental education and low personal education…Structural amplification condemns some families to the concentration of low education with poor health across generations… Break that mediating link, and the moderating effect of higher education will suppress the health disadvantages of the socially disadvantaged origins. ”
High Societal Price in Health of Education Forgone
An estimate of the number of annual deaths attributable to lack of high school education among persons 25–64 years of age in the United States (237,410) exceeds the number of deaths attributed to cigarette smoking among persons 35–64 years of age (163,500) (Krueger et al., unpublished manuscript, 2013). 56 (The estimate of smoking-attributable mortality does not include adults younger than 35 years of age because mortality from smoking is negligible at this age.)
Several recent estimates have been made of economic costs to individuals, the government, and society of the failure of each American to achieve an optimal education. Although it may be argued that there is a moral duty to redress injustice and inequity regardless of cost, these estimates indicate the economic magnitude of this loss and the potential value of its redress.
Schoeni and colleagues 57 , 58 estimate the annual economic value of health forgone in the United States in 2006 by adults who lack a college education. For a population of 138 million aged 25 years or older with less than a college education, the economic value of the life and health forgone is US$1.02 trillion per year – 7.7% of US gross domestic product.
Levin and colleagues 59 provide an estimate of benefits to the government (in 2004 dollars) if those who did not finish high school had completed a high school education (or higher) with a diploma. Based on governmental benefits of income taxes associated with greater earnings of high school graduates and reduced costs of welfare and incarceration, Medicaid, and lifetime savings of approximately US$40,000 per capita in public health expenses, they estimated a total lifetime benefit of US$209,000 for each high school dropout if he or she had instead completed high school. They then examined the costs and benefits of 5 programs with demonstrated efficacy in improving rates of high school completion. Cost–benefit ratios range from 1.5 to 3.5, indicating substantial governmental benefit. 59
Education as a Domain of Public Health Action
Just as many areas of daily life are recognized domains of legitimate public health action – agriculture (eg, nutrition and food safety), transportation (eg, vehicle injuries, air pollution, and walking), immigration (eg, immigrant health and infection control), justice (eg, violent crime and prison health), urban design (eg, safety, walkable communities, and food deserts), and labor (eg, occupational safety and health) – so should education (beyond health education in schools) be recognized as a legitimate domain of public health action. Education is a critical component of health and, we argue, education is a major, long-term, multifaceted cause of health. In particular, education is a powerful means of breaking the cycle of poverty (which greatly affects ethnic and racial minority populations) and promoting health equity.(As this article was in press, the authors encountered an excellent paper by Cohen and Syme 60 which draws similar conclusions.)
Several federal agencies have supported “health in all policies,” 61 particularly through the National Prevention, Health Promotion and Public Health Council. 62 The US Department of Health and Human Services includes in its mission 63 to “engage multiple sectors to take actions to strengthen policies and improve practices that are driven by the best available evidence and knowledge” and in its overarching goals to “Create social and physical environments that promote good health for all.”
States and the District of Columbia have also adopted a “health in all policies” perspective. California’s “CAL Health in all Policies” 64 – 66 recognizes the potential for education as a means of moving toward health equity. “Promote efforts that demonstrate positive effects in closing the achievement gap. Collaborate on advancing strategies, addressing the major factors that inhibit the learning of all students.” Counties (eg, Los Angeles, Baltimore) also have adopted a “health in all policies” perspective. 64 , 67 , 68
The effort to pursue multi-sectoral strategies for health improvement is international, practiced in the European Union, Australia, and elsewhere. The European Union has adopted a social determinants-based approach: “Health in All Policies addresses the effects on health across all policies such as agriculture, education, the environment, fiscal policies, housing, and transport. It seeks to improve health and at the same time contribute to the well-being and the wealth of the nations through structures, mechanisms, and actions planned and managed mainly by sectors other than health.” 69 (pXVIII)
In “A Framework for Public Health Action: The Health Impact Pyramid,” 71 Frieden writes, “Interventions that address social determinants of health have the greatest potential public health benefit” and contrasts social determinants – the base of the “health impact pyramid” – with higher strata in the pyramid. 70 (p594) Among social determinants, education is fundamental, because education forms the new members of society – children and youth. Effective teachers are facilitators of long-term health benefits. Beyond school health promotion, education as a means of public health intervention is more difficult to define, to administer, to measure, and to evaluate. It is cumulative, formative, and transformative, both for the individuals who experience it and for the society it recreates and modifies. Although these features make education more challenging than some other tools of public health, such challenges must not deter the public health community from working closely with the education community to investigate and understand this form of social determinant causation, evaluate the wide array of educational program types, and mobilize for action on this powerful force for public health benefits.
Acknowledgments
Many thanks to thoughtful readers and editors Randy Elder, Catherine Ross, Barbara Rimer, Kate W. Harris, Amy Brown, Heba Athar, and Kristen Folsom.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biographies
Robert A. Hahn received his PhD in anthropology at Harvard University (1976) and his MPH in epidemiology from the University of Washington (1986). Since 1986, he has served as an epidemiologist at the US Centers for Disease Control and Prevention (CDC) in Atlanta and is a member of the Senior Biomedical Research Service. He is the author of Sickness and Healing: An Anthropological Perspective (1995) and co-editor of Anthropology and Public Health: Bridging Differences in Culture and Society (2008), with a second edition recently published. In 1998–1999, he worked as a Capitol Hill Fellow in the US House of Representatives Committee on Veterans Affairs and in the office of Congresswoman Louise Slaughter. He is currently coordinating scientist of systematic reviews on health equity for the CDC Guide to Community Preventive Services .
Benedict I. Truman earned his BS in chemistry and MD from Howard University and his MPH from the Johns Hopkins Bloomberg School of Public Health, where he completed a residency in preventive medicine and public health and served as chief resident. He has held scientific and leadership positions in state, local, and federal public health agencies and is the associate director for science at the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at the US Centers for Disease Control and Prevention (CDC). In this role, he works with other scientists and program managers to ensure that the CDC’s scientific products and research ethics meet the highest standards of quality and integrity. He has published many peer-reviewed journal articles on educational interventions for health equity; prevention and control of infectious diseases and chronic noninfectious diseases; adolescent and school health; community preventive services guidelines; minority health and health disparities; employee performance and public health workforce development; and applied epidemiologic methods. He serves as the Consulting Editor for Infectious Diseases for the Journal of Public Health Management and Practice .
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
- 1. Dewey J. Democracy and Education: An Introduction to the Philosophy of Education. New York, NY: MacMillan Co; 1916. [ Google Scholar ]
- 2. Silva E. [Accessed May 9, 2014];On the clock: rethinking the way schools use time. 2007 http://www.educationsector.org/publications/clock-rethinking-way-schools-use-time .
- 3. Bandura A. Social Learning Theory. New York, NY: General Learning Press; 1977. [ Google Scholar ]
- 4. Feinstein L, Sabates R, Anderson TM, Sorhaindo A, Hammond C. What are the Effects of Education on Health?. Copenhagen, Denmark. Measuring the Effects of Education on Health and Civic Engagement: Proceedings of the Copenhagen Symposium, OECD; 2006. [ Google Scholar ]
- 5. Basch CE. Healthier Students Are Better Learners: A Missing Link in School Reforms to Close the Achievement Gap. Equity Matters. 2010 doi: 10.1111/j.1746-1561.2011.00632.x. Research Review No. 6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Peters LW, Kok G, Ten Dam GT, Buijs GJ, Paulussen TG. Effective elements of school health promotion across behavioral domains: a systematic review of reviews. BMC Public Health. 2009;9:182–195. doi: 10.1186/1471-2458-9-182. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Rasberry C, Lee SM, Robin L, et al. The association between school-based physical activity, including physical education, and academic performance: a systematic review of the literature. Prev Med. 2011;52(Suppl 1):S10–S20. doi: 10.1016/j.ypmed.2011.01.027. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Ross CE, Wu CL. The links between education and health. Am Soc Rev. 1995;60(5):719–745. [ Google Scholar ]
- 9. World Health Organization. [Accessed May 9, 2014];Declaration of Alma-Ata. 1978 http://www.who.int/publications/almaata_declaration_en.pdf?ua=1 .
- 10. Egerter S, Braveman P, Sadegh-Nobari T, Grossman-Kahn R, Dekker M. Education matters for health. Educ Health. 2009;6:1–15. [ Google Scholar ]
- 11. Bradberry T, Greaves J. Emotional Intelligence 2.0. San Diego, CA: Talent Smart; 2009. [ Google Scholar ]
- 12. Mirowsky J, Ross CE. Education, learned effectiveness and health. London Rev Educ. 2005;3:205–220. [ Google Scholar ]
- 13. National Commission on Excellence in Education. A Nation at Risk. Washington DC: U.S. Government Printing Office; 1983. [ Google Scholar ]
- 14. Secretary’s Commission on Achieving Necessary Skills. A SCANS report for America. 2000. Learning a living: a blueprint for high performance. [ Google Scholar ]
- 15. CDC Healthy Aging Program. [Accessed May 9, 2014];The CDC Healthy Brain Initiative: Progress 2006–2011. 2011 http://www.cdc.gov/aging/healthybrain .
- 16. National Institutes of Health. [Accessed May 5, 2014];Healthy Brain Initiative. http://trans.nih.gov/cehp/
- 17. Sadana R, Tandon A, Murray CLJ, et al. Describing population health in six domains: comparable results from 66 household surveys. Global Programme on Evidence for Health Policy. Discussion Paper No. 43. Geneva, Switzerland: WHO; 2002. [ Google Scholar ]
- 18. U.S. Congress, Office of Technology Assessment. Testing in American Schools: Asking the Right Questions, OTA-SET-519. Washington DC: U.S. Government Printing Office; 1992. [ Google Scholar ]
- 19. Bowers A. Reconsidering grades as data for decision making: more than just academic knowledge. J Educ Admin. 2009;47:609–629. [ Google Scholar ]
- 20. Willingham W, Pollack JM, Lewis C. Grades and test scores: accounting for observed differences. J Educ Meas. 2002;39:1–37. [ Google Scholar ]
- 21. Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [ Google Scholar ]
- 22. Powell KE, Spain KG, Christenson GM, Mollenkamp MP. The status of the 1990 objectives for physical fitness and exercise. Public Health Rep. 1986;101(1):15–21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. U.S. Department of Health and Human Services. Physical Activity and Health: a Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [ Google Scholar ]
- 24. Karhausen LR. Causation: the elusive grail of epidemiology. Med, Health Care Philos. 2000;3:59–67. doi: 10.1023/a:1009970730507. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Bradford-Hill A. The environment and disease: association or causation? Proc Royal Soc Med. 1965;58:295–300. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Susser M. Causal Thinking in the Health Sciences. Concepts and Strategies of Epidemiology. New York, NY: Oxford University Press; 1973. [ Google Scholar ]
- 27. CDC Division of Adolescent and School Health. [Accessed May 5, 2014];Health-risk behaviors and academic achievement. 2009 http://www.cdc.gov/healthyyouth/health_and_academics/pdf/health_risk_behaviors.pdf .
- 28. Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Winkelby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–820. doi: 10.2105/ajph.82.6.816. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Murnane RJ. Improving the education of children living in poverty. Future Child. 2007;17:161–182. doi: 10.1353/foc.2007.0019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Chetty R, Friedman JN, Hilger N, et al. How does your kindergarten classroom affect your earnings? Evidence from Project Star. Q J Econ. 2011;126(4):1593–1660. doi: 10.1093/qje/qjr041. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Ferraro KF, Farmer MM. Utility of health data from social surveys: is there a gold standard for measuring morbidity? Am Sociol Rev. 1999;64(2):303–315. [ Google Scholar ]
- 33. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty seven studies community. J Health Soc Behav. 1997;38:21–37. [ PubMed ] [ Google Scholar ]
- 34. Prus SG. Comparing social determinants of self-rated health across the United States and Canada. Soc Sci Med. 2011;73:50–59. doi: 10.1016/j.socscimed.2011.04.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Schiller JS, Lucas JW, Ward BW, Peregoy JA National Center for Health Statistics. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10(252):1–207. [ PubMed ] [ Google Scholar ]
- 36. Ross CE, Wu CL. Education, age and the cumulative advantage in health. J Health Soc Behav. 1996;37:104–120. [ PubMed ] [ Google Scholar ]
- 37. CDC National Center for Health Statistics. Health, United States, 2008. Hyattsville, MD: National Center for Health Statistics; 2009. [ Google Scholar ]
- 38. Rostron BL, Boies JL, Arias E National Center for Health Statistics. Education reporting and classification on death certificates in the United States. Vital Health Stat. 2010;2(151):1–19. [ PubMed ] [ Google Scholar ]
- 39. Muennig P, Schweinhart L, Montie J, Neidell M. Effects of a prekindergarten educational intervention on adult health: 37-year follow-up results of a randomized controlled trial. Am J Public Health. 2008;99(8):1431–1437. doi: 10.2105/AJPH.2008.148353. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Ramey C, Campbell FA, Burchinal M, et al. Persistent effects of early childhood education on high-risk children and their mothers. Appl Dev Sci. 2000;4:2–14. [ Google Scholar ]
- 41. Muennig P, Robertson D, Johnson G, et al. The effect of an early education program on adult health: the Carolina Abecedarian project randomized controlled trial. Am J Public Health. 2011;101:512–516. doi: 10.2105/AJPH.2010.200063. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Campbell F, Conti G, Heckman JJ, et al. Early childhood investments substantially boost adult health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Reynolds AJ, Temple JA, Ou SR, et al. Effects of a school-based, early childhood intervention on adult health and well-being: a 19-year follow-up of low-income families. Arch Pediatr Adolesc Med. 2007;161:730–739. doi: 10.1001/archpedi.161.8.730. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Barnett WS. Effectiveness of early educational intervention. Science. 2011;333:975–978. doi: 10.1126/science.1204534. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Lleras-Muney A. The relationship between education and adult mortality in the United States. Rev Econ Stud. 2005;72:189–221. [ Google Scholar ]
- 46. Lochner L, Moretti R. The effect of education on crime: evidence from prison inmates, arrests, and self-reports. Am Econ Rev. 2004;94:155–189. [ Google Scholar ]
- 47. Black SE, Devereux PJ, Salvanes KG. Fast times at Ridgemont High? The effect of compulsory schooling laws on teenage births. [Accessed May 9, 2014];NBER Working Paper Series: Working Paper 10911. 2004 http://www.nber.org/papers/w10911 .
- 48. Arendt JN. Does education cause better health? A panel data analysis using school reforms for identification. Econ Educ Rev. 2005;24:149–160. [ Google Scholar ]
- 49. Gottfredson LS. Intelligence: is it the epidemiologists’ elusive fundamental cause of social class inequalities in health? J Pers Soc Psychol. 2004;86(1):174–199. doi: 10.1037/0022-3514.86.1.174. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Link BG, Phelan JC, Miech R, Westin EL. The resources that matter: fundamental social causes of health disparities and the challenge of intelligence. J Health Soc Behav. 2008;49(1):72–91. doi: 10.1177/002214650804900106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Winship C, Korenman S. Does staying in school make you smarter: the effect of education on IQ in the Bell Curve. In: Devlin B, Fienberg SE, Resnick DP, Roeder K, editors. Intelligence, Genes, and Success. Scientists Respond to The Bell Curve. New York, NY: Springer Verlag; 1997. [ Google Scholar ]
- 52. World Health Organization. Closing the gap in a generation: health equity through action on the social determinants of health. [Accessed May 9, 2014];Final Report of the Commission on Social Determinants of Health. 2008 http://www.who.int/social_determinants/thecommission/finalreport/en/index.html .
- 53. Ross CE, Mirowsky J. Refining the association between education and health: the effects of quantity, credential, and selectivity. Demography. 1999;36:445–460. [ PubMed ] [ Google Scholar ]
- 54. Reynolds JR, Ross CE. Social stratification and health: education’s benefit beyond economic status and social origins. Soc Probl. 1998;45(2):221–247. [ Google Scholar ]
- 55. Ross CE, Mirowsky J. The interaction of personal and parental education on health. Soc Sci Med. 2011;72:591–599. doi: 10.1016/j.socscimed.2010.11.028. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Office of the Surgeon General. The Health Consequences of Smoking—50 years of Progress. A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2014. [ Google Scholar ]
- 57. Schoeni R, Dow WF, Miller WD, Pamuk ER. The economic value of improving the health of disadvantaged Americans. Am J Prev Med. 2011;40(1Suppl1):S67–S72. doi: 10.1016/j.amepre.2010.09.032. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Rothwell J. Metropolitan Policy Program: Brookings Institution. 2012. Housing Costs, Zoning, and Access to High-Scoring Schools. [ Google Scholar ]
- 59. Levin H, Belfield C, Muennig P, Rouse C. [Accessed September 5 2014];The Costs and Benefits of an Excellent Education for all of America’s Children. 2006 http://www.irre.org/publications/costs-and-benefits-excellent-education-all-americas-children .
- 60. Cohen AK, Syme SL. Education: a missed opportunity for public health intervention. Am J Public Health. 2013;103(6):997–1001. doi: 10.2105/AJPH.2012.300993. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Healthy People. [Accessed May 9, 2014];Social Determinants of Health. 2020 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39 .
- 62. National Prevention Health Promotion and Public Health Council. [Accessed May 9, 2014];2010 Annual Status Report. 2010 http://www.hhs.gov/news/reports/nationalprevention2010report.pdf .
- 63. US Department of Health and Human Services. [Accessed May 9, 2014];Healthy People 2020. 2010 http://www.healthypeople.gov/2020/default.aspx .
- 64. Fielding JE. [Accessed May 9, 2014];Health in All Policies: Lessons Learned by LA County DPH. http://publichealth.lacounty.gov/docs/Fielding%20CDC%20L2L%207.8.08%20-%20FINAL.pdf .
- 65. Gase LN, Pennotti R, Smith KD. Health in all policies: taking stock of emerging practices to incorporate health in decision making in the United States. J Public Health Manag Pract. 2013;19(6):529–540. doi: 10.1097/PHH.0b013e3182980c6e. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. National Association of County and City Health Officials. [Accessed May 9, 2014];Health in All Policies. http://www.naccho.org/topics/environmental/HiAP/
- 67. Baltimore City Health Department. [Accessed May 9, 2014];Healthy Baltimore. http://www.baltimorehealth.org/healthybaltimore2015.html .
- 68. Rudolph L, Caplan J, Ben-Moshe K, Dillon L. Health in All Policies: A Guide for State and Local Governments. Washington, DC and Oakland, CA: American Public Health Association and Public Health Institute; 2013. [ Google Scholar ]
- 69. Ståhl T, Wismar M, Ollila E, Lahtinen E, Leppo K, editors. [Accessed May 9, 2014];Health in All Policies Prospects and Potentials. 2006 http://www.euro.who.int/__data/assets/pdf_file/0003/109146/E89260.pdf .
- 70. Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–595. doi: 10.2105/AJPH.2009.185652. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (532.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Click here - to use the wp menu builder

- Privacy Policy
- Refund Policy
- Terms Of Service
- Nursing notes PDF
- Nursing Foundations
- Medical Surgical Nursing
- Maternal Nursing
- Pediatric Nursing
- Behavioural sciences
- BSC NURSING
- GNM NURSING
- MSC NURSING
- PC BSC NURSING
- HPSSB AND HPSSC
- Nursing Assignment
The 10 Importance of Health Education
Importance of Health Education – Health education is important for individuals, families, and communities. It can help people learn about their health, make healthy choices, and reduce their risk of disease. Health education plays a crucial role in improving individual and community well-being. It encompasses the dissemination of knowledge and information to promote healthy lifestyles, prevent diseases, and enhance the overall quality of life. Here are 10 importance of health education.
Table of Contents
What is Health Education and Why is it important?
Health education is the process of providing knowledge and skills to promote good health. It’s important because it empowers individuals to prevent illness, adopt healthy behaviors, and make informed decisions about their well-being. It covers various topics, from disease prevention to mental health awareness, and helps create healthier communities while reducing healthcare costs.
Benefits of Health Education
When you embrace health education, you open the door to a host of benefits. First and foremost, it enhances your understanding of your body and mind. You’ll learn how to identify warning signs, spot the red flags, and take action before issues escalate. Moreover, it’s the secret to a longer, happier life. With the right knowledge, you can reduce the risk of chronic diseases, live with vitality, and enjoy your golden years to the fullest.
Definition of health education
Health education is the process of imparting knowledge and skills related to health and well-being. It aims to empower individuals with the information they need to make informed decisions about their health and adopt positive behaviors that contribute to overall wellness.
Here are 10 importance of health education:
Promotes Disease Prevention
One of the primary objectives of health education is to prevent diseases. By educating people about healthy practices, such as maintaining proper hygiene, exercising regularly, and having a balanced diet , health education can significantly reduce the risk of various illnesses and health conditions.
Empowers Individuals to Make Informed Decisions
Informed decision-making is vital for personal health management. Health education equips individuals with the necessary knowledge to assess health-related choices critically. This empowers them to make informed decisions about medical treatments, lifestyle changes, and preventive measures.
Encourages Healthy Behaviors
Health education inspires the adoption of healthy behaviors. When people are aware of the benefits of good habits like regular exercise, avoiding smoking, and excessive alcohol consumption, they are more likely to embrace these positive changes for a healthier life.
Reduces Healthcare Costs
Preventive measures encouraged through health education can lead to a significant reduction in healthcare costs. By preventing diseases and promoting healthier lifestyles, the burden on healthcare systems decreases, allowing resources to be allocated more efficiently.
Fosters a Healthier Society
A society that prioritizes health education experiences improved overall well-being. It creates a community that supports and encourages healthy choices, leading to a positive and productive environment for everyone.
Addresses Mental Health and Well-being
Health education isn’t limited to physical health; it also encompasses mental health. By promoting awareness about mental health issues and providing support systems, health education contributes to reducing the stigma surrounding mental health and improving overall well-being.
Improves the Quality of Life
When individuals take charge of their health through education and informed decision-making, they experience an enhanced quality of life. Good health positively impacts various aspects of life, including relationships, careers, and overall happiness.
Health Education in Schools and Communities
Schools and communities play a pivotal role in promoting health education . Integrating health education into school curriculums and community programs ensures that individuals receive the necessary information from an early age, establishing a foundation for lifelong healthy habits.
Health Education for a Sustainable Future
Health education is vital for creating a sustainable future. By raising awareness about environmental issues, healthy living, and responsible consumption, health education contributes to a greener, more sustainable planet.
10 importance of health education in schools
Health education in schools plays a crucial role in promoting overall well-being and empowering students to make informed decisions about their health. Here are ten important reasons why health education in schools is essential:
- Promotes Healthy Behavior: Health education equips students with knowledge about nutrition, physical activity, and hygiene, encouraging them to adopt healthy lifestyle choices.
- Disease Prevention: It educates students about common diseases, their causes, and prevention strategies, reducing the risk of illness.
- Sexual Education: Provides essential information about sexual health, safe practices, and contraceptive methods to reduce the risk of unwanted pregnancies and sexually transmitted infections.
- Mental Health Awareness: Helps students recognize signs of mental health issues, reducing stigma, and encouraging seeking help when needed.
- Substance Abuse Prevention: Teaches about the dangers of drug and alcohol abuse, promoting responsible behavior and addiction prevention.
- Healthy Relationships: Educates students about healthy communication, consent, and building positive relationships while preventing abusive behavior.
- Safety Awareness: Teaches safety measures, first aid, and emergency response, ensuring students are prepared for unexpected situations.
- Nutrition and Diet: Provides knowledge about balanced diets, portion control, and food choices, reducing the risk of obesity and related health issues.
- Stress Management: Equips students with coping strategies for stress, anxiety, and emotional challenges, promoting mental resilience.
- Lifelong Skills: Imparts life skills such as decision-making, problem-solving, and critical thinking, which are essential for making informed health choices throughout life.
Aims and objectives of health education
The aims and objectives of health education are to:
- Increase health knowledge: Understand the body, its functioning, and how to maintain good health.
- Encourage healthy behaviors: Adopt a balanced diet, regular exercise, sufficient sleep, and avoid smoking and excessive alcohol consumption.
- Prevent diseases: Learn about specific risk factors and modify your lifestyle accordingly.
- Promote self-care: Equip individuals to manage their health and access necessary healthcare services.
- Empower individuals: Teach patients’ rights and self-advocacy for better health outcomes.
- Create supportive environments: Advocate for policies promoting healthy living, including nutritious food and physical activity.
The Purpose of Health Education in Nursing
Health education is a crucial component of nursing practice. It is the process of providing patients and communities with the knowledge, skills, and support they need to make informed decisions about their health and well-being.
Health education in nursing plays a number of important roles, including:
- Promoting health and preventing illness. Health education empowers individuals to adopt healthy behaviors, make lifestyle changes, and take preventive measures to avoid illness and disease. By providing information about risk factors and healthy habits, nurses can help people lead healthier lives.
- Enhancing patient understanding. Nurses educate patients about their medical conditions, treatment options, and medications. This helps patients understand their health conditions better, adhere to prescribed treatments, and actively participate in their care.
- Improving self-management. For patients with chronic illnesses, health education equips them with the skills needed to manage their conditions effectively. This may include teaching them about symptom management, monitoring techniques, and when to seek medical help.
- Empowering patients. Health education empowers patients to take charge of their own health. Nurses provide them with knowledge and tools to make informed decisions, enabling them to be active partners in their healthcare journey.
- Supporting healthy lifestyles. Nurses promote healthy habits, such as proper nutrition, regular exercise, stress management, and adequate sleep. By educating patients about these lifestyle factors, nurses encourage the prevention of chronic diseases and overall well-being.
- Addressing health disparities. Health education can target specific populations or communities that may face health disparities. By tailoring education to their unique needs, nurses can work towards reducing health inequalities.
- Community health promotion. Nurses engage in health education at the community level to address public health concerns, raise awareness about prevalent health issues, and promote health initiatives that benefit the entire community.
- Facilitating recovery and rehabilitation. Health education supports patients during the recovery and rehabilitation process, helping them understand post-treatment care, medications, and lifestyle adjustments to optimize their recovery outcomes.
Conclusion -Importance of Health Education
In conclusion, health education is an indispensable aspect of our society. By promoting disease prevention, empowering individuals to make informed decisions, and encouraging healthy behaviors, health education significantly improves individual and community well-being. It addresses physical and mental health, reduces healthcare costs, and fosters a healthier and more sustainable future.
FAQs -Importance of Health Education
What is health education.
Health education is the process of imparting knowledge and skills related to health and well-being to empower individuals to make informed decisions about their health.
How does health education promote disease prevention?
Health education disseminates information about healthy practices, which helps in reducing the risk of various diseases and health conditions.
Why is health education crucial in schools and communities?
Integrating health education in schools and communities ensures that individuals receive the necessary information from an early age, establishing a foundation for lifelong healthy habits.
Please note that this article is for informational purposes only and should not substitute professional medical advice.
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Recent articles
Scope of nursing profession, itbp head constable midwife anm recruitment 2023: apply now, the principles of health education, stages sign and symptoms of labour, a comprehensive guide to physical assessment in nursing, modes of communication in nursing, download nursing notes pdf, male and female reproductive system pdf, mental health psychiatric notes, human skeletal system nursing, psychology note nursing pdf, medical surgical nursing- nursing assignment on dialysis, national health programmes in india pdf, mental health nursing history collection, anatomy and physiology of female reproductive system, more like this, gifts for nursing home residents, gift ideas for nursing students, crystalloid and colloid: differences and when to use each, how to insert a catheter in a female patient -female catheterization, mental health nursing diagnosis care plan pdf, child pediatric health nursing notes -bsc nursing, mid-wifery pdf notes for nursing students, reproductive system nursing notes pdf, primary health care nursing notes pdf, nursingenotes.com.
- STUDY NOTES
- SUBJECT NOTES
A Digital Platform For Nursing Study Materials
Latest Articles
Most popular.
© Nursingenotes.com | All rights reserved |

Online Students
For All Online Programs
International Students
On Campus, need or have Visa
Campus Students
For All Campus Programs
The Importance of Health Education

Understanding the Numbers When reviewing job growth and salary information, it’s important to remember that actual numbers can vary due to many different factors — like years of experience in the role, industry of employment, geographic location, worker skill and economic conditions. Cited projections do not guarantee actual salary or job growth.
When it comes to building a healthy community, the importance of health education cannot be overlooked. Community health workers collaborate with all stakeholders in a community — from its citizens to its government, education and medical officials — to improve health and wellness and ensure equal access to healthcare.
First, What is Health Education?
According to the World Health Organization (WHO), health education is a tool to improve a population's general health and wellness through promoting knowledge and healthy practices ( WHO PDF source ).
Although the subject is often taught in school settings, students aren't the only ones who need to know about health. In fact, all age groups and demographics can benefit from health education.
Why is Health Education Important?
Community health education looks at the health of a community as a whole, seeking to identify health issues and trends within a population and work with stakeholders to find solutions to these concerns.
The importance of health education impacts many areas of wellness within a community, including:
- Chronic disease awareness and prevention
- Injury and violence prevention
- Maternal and infant health
- Mental and behavioral health
- Nutrition, exercise and obesity prevention
- Tobacco use and substance abuse
Community health educators work with public health departments, schools, government offices and even local nonprofits to design educational programs and other resources to address a community’s specific needs.
“As public health professionals, with aid of community leaders, we strive to ensure community wellness as it pertains to health education,” said Dr. Tanyi Obenson .
Obenson is a public health clinical faculty member at Southern New Hampshire University (SNHU) who holds a PhD in Public Health. “A healthier community is a better community,” he said.
How Does Health Education Impact a Community?
Health education can impact communities by addressing relevant issues and concerns at a local level. For example:
Healthcare Disparities

In addition to providing educational resources and programming to a community, public health educators also work to ensure all members of a community have equal access to wellness resources and healthcare services.
“When considering care access and delivery within communities, health equity and social justice are one in the same,” said Dr. Natalie Rahming , an adjunct healthcare faculty member at SNHU with almost two decades of experience working in the healthcare field. “The social determinants of health classify the various ways in which an individual’s identity characteristics and social positions are woven into a fabric of discrimination.”
According to Rahming, common health disparities include:
- Gender health disparities
- Racial or ethnic health disparities
- Rural and urban health disparities
- Socioeconomic health disparities
Rahming said racism and other disparities have manifested into unequal distribution of care across distinct groups over many generations.
“A community health worker seeks to abolish or ameliorate health inequity from a social lens, whereas other health care workers approach it at an individual perspective,” she said. “Both are critical for healthcare advancement.”
Community Health Education and Government Policy
The importance of health education also extends into policy and legislation development at a local, state and national level, informing and influencing key decisions that impact community health.
From campaigns and legislation to enforce seat belt use and prevent smoking to programs that boost the awareness and prevention of diabetes, public health workers provide research and guidance to inform policy development.

“The collaboration of community leaders is essential to form a shared commitment and results-oriented approach to improving the health of our most vulnerable populations,” she said.
The Economic Importance of Health Education
Health education can also boost a community’s economy by reducing healthcare spending and lost productivity due to preventable illness.
Obesity and tobacco use, for example, cost the United States billions of dollars each year in healthcare costs and lost productivity.
According to the National Collaborative on Childhood Obesity (NCCOR), the annual loss in economic productivity due to obesity and related issues is expected to total as much as $580 billion by 2030 ( NCCOR PDF source ). The total economic cost of tobacco use costs the United States more than $300 billion each year, including $156 billion in lost productivity , according to the CDC.
Programs designed to help community members combat expensive health issues not only boost individuals’ health but also provide a strong return on investment for communities.
According to the CDC, states with strong tobacco control programs see a $55 return on every $1 investment , mostly from avoiding costs to treat smoking-related illness. The national cost of offering the National Diabetes Prevention Program is about $500 per participant , significantly lower than the $9,600 spent on diabetes care per type 2 diabetes patient each year.
Find Your Program
How to become a community healthcare worker.
A community healthcare worker's goal is to help others, starting with education.
To begin your career in community healthcare, you'll typically need a minimum of a high school diploma or associate degree . The work done within public health and community healthcare differs from other healthcare fields and impacts communities in different ways requiring different training and understanding of healthcare.
“Unlike individual healthcare delivery, public health investigates the systems and trends that impact behaviors and outcomes within a community collectively," said Rahming. “This research facilitates the identification of needs and provision of tools to promote disease prevention, individual empowerment, and improved wellness that enhances the quality of life for all."
Earning your bachelor's degree in public health or community health could help you advance your career and better understand your work. On top of your classroom education, many community health care workers are required to complete on-the-job training. According to BLS, training often covers communication, outreach, and information based upon your specific community health focus.
Public Health Education: A Growing Field
As the health, social and economic impacts of community health education continue to grow, so does the field of public health and health promotion.
According to the U.S. Bureau of Labor Statistics (BLS), the role of health education specialist is projected to grow by 7% through 2032, faster than the average for all occupations.*
BLS said that health education specialists usually need a bachelor's degree but that some health education specialist jobs require you to have a master's degree, too.
Earning your Master of Public Health (MPH) degree could be a proactive way to expand your knowledge and prepare for a career in the public health education field. Whether you want to be a health education specialist or an epidemiologist, there are a variety of things you can do with your MPH . You can also focus your MPH studies on specific areas, such as global health, by adding a concentration to your degree.
When considering MPH programs, look for one accredited by the Council on Education for Public Health ( CEPH ), such as SNHU's. CEPH is an independent agency recognized by the U.S. Department of Education, and their accreditation means that the program has met the standards.
In an accredited MPH program, you can gain the skills you need to lead illness and disease prevention efforts, build community wellness programs and advocate for public health policy.
Whether you decide to pursue an MPH or community health education degree, the public health education field has a wide variety of settings where you may work. According to BLS, these settings include:
- Government organizations and public health departments
- Hospitals and healthcare facilities
- Nonprofit organizations
- Private businesses and employee wellness programs
- Schools and colleges

“I believe that more and more communities are seeing benefits from wellness-related initiatives and receiving positive marks about them,” Gifford said. “Hence, community leaders are seeing this as not just a business-driven necessity, but also something that impacts the well being and quality of life of their citizens.”
Discover more about SNHU’s bachelor's in community health : Find out what courses you'll take, skills you’ll learn and how to request information about the program.
*Cited job growth projections may not reflect local and/or short-term economic or job conditions and do not guarantee actual job growth. Actual salaries and/or earning potential may be the result of a combination of factors including, but not limited to: years of experience, industry of employment, geographic location, and worker skill.
Danielle Gagnon is a freelance writer focused on higher education. She started her career working as an education reporter for a daily newspaper in New Hampshire, where she reported on local schools and education policy. Gagnon served as the communications manager for a private school in Boston, MA before later starting her freelance writing career. Today, she continues to share her passion for education as a writer for Southern New Hampshire University. Connect with her on LinkedIn .
Explore more content like this article


Academic Spotlight: Health Professions Executive Director Dr. Toni Clayton

What Are the Different Levels of Nursing Degrees?

Looking Forward in Healthcare at SNHUs 4th Annual Global Summit
About southern new hampshire university.

SNHU is a nonprofit, accredited university with a mission to make high-quality education more accessible and affordable for everyone.
Founded in 1932, and online since 1995, we’ve helped countless students reach their goals with flexible, career-focused programs . Our 300-acre campus in Manchester, NH is home to over 3,000 students, and we serve over 135,000 students online. Visit our about SNHU page to learn more about our mission, accreditations, leadership team, national recognitions and awards.
The Knowledge Hub
Unlocking the power of information
The Benefits of Health Education: Exploring Its Role in Public Health and Healthcare Delivery

Introduction
Health education is an important component of the public health system. It involves the dissemination of information and skills that enable individuals to make informed decisions about their health. Health education can be used to promote healthy behaviors, prevent disease, reduce health disparities, and improve access to health care. In this article, we will explore the benefits of health education, examine its role in society, and investigate how technology is changing health education.
Exploring the Benefits of Health Education
Health education has many benefits, including improved quality of life, increased awareness of health issues, and improved access to health care. Let’s take a closer look at these benefits.
Improved Quality of Life
Health education can lead to improved quality of life by teaching people about proper nutrition, physical activity, and other lifestyle behaviors that can help them maintain good health. By providing accurate information about health-related topics, health education can also help people make better decisions about their health, leading to healthier lifestyles.
Increased Awareness of Health Issues
Health education can also increase awareness of health issues, such as the importance of regular check-ups, the dangers of smoking, and the need to get immunized. This increased awareness can help people take steps to maintain their health and seek medical attention when necessary.
Improved Access to Health Care
By providing information about health care services, health insurance, and other resources, health education can help people gain access to the health care they need. In addition, health education can help people understand their rights and responsibilities as patients, which can lead to better communication with health care providers and improved outcomes.

Examining the Role of Health Education in Society
Health education plays an important role in promoting health and preventing disease. It can be used to encourage healthy habits and behaviors, such as exercising regularly, eating a balanced diet, and getting regular check-ups. It can also be used to raise awareness about health-related issues and educate people about how to prevent illness and injury.
Promotion of Healthy Habits and Behaviors
Health education can be used to promote healthy habits and behaviors, such as exercise, healthy eating, and stress management. By providing accurate information and skills, health education can help people make better decisions about their health, leading to healthier lifestyles.
Prevention of Disease and Illness
Health education can also be used to raise awareness about health-related issues and teach people how to prevent diseases and illnesses. For example, health education can provide information about the dangers of smoking, the importance of immunization, and the need to practice safe sex.
Engagement of Communities in Health Promotion
Health education can also be used to engage communities in health promotion. By providing health education programs, community organizations can help people become more aware of health issues, learn healthy habits and behaviors, and gain access to health care.
An Overview of Health Education Programs
Health education programs are designed to meet the needs of specific populations. They typically include a variety of activities, such as lectures, workshops, and hands-on activities. The goals and objectives of health education programs vary, depending on the needs of the target population. Health education programs can use a variety of delivery methods, including face-to-face instruction, online learning, and multimedia.
Types of Programs
Health education programs can be tailored to meet the needs of different populations. For example, there are programs for children, adolescents, adults, and seniors. There are also programs for different cultures and ethnicities, and programs for people with special needs.
Goals and Objectives
The goals and objectives of health education programs vary, depending on the needs of the target population. Common goals include improving knowledge and skills related to health, changing attitudes and behaviors related to health, and increasing access to health care.
Delivery Methods
Health education programs can use a variety of delivery methods. Face-to-face instruction is a common method, but other methods include online learning, multimedia, and print materials. These methods can be used alone or in combination to reach a wider audience.
Investigating the Impact of Health Education on Public Health
Health education has a significant impact on public health. It can be used to inform policy development, reduce health disparities, and improve health outcomes. Let’s take a closer look at these impacts.
Effects on Policy Development
Health education can play an important role in informing policy development. By providing accurate information about health-related topics, health education can help policymakers identify and address health issues, develop effective policies, and allocate resources to support health initiatives.
Reduction of Health Disparities
Health education can also be used to reduce health disparities. By providing information about health care services, health insurance, and other resources, health education can help vulnerable populations gain access to the health care they need.
Improved Health Outcomes
Finally, health education can lead to improved health outcomes. By teaching people about proper nutrition, physical activity, and other lifestyle behaviors, health education can help people make better decisions about their health, leading to healthier lifestyles and better health outcomes.
Understanding the History and Evolution of Health Education
Health education has a long and rich history. From its early beginnings in the 19th century to its modern developments in the 21st century, health education has evolved to meet the changing needs of society. Let’s take a look at the history and evolution of health education.
Early Beginnings
Health education began in the 19th century, with the establishment of public health campaigns to promote hygiene and prevent the spread of disease. As public health concerns shifted from infectious diseases to lifestyle-related diseases, health education began to focus on promoting healthy habits and behaviors.
Modern Developments
In the 20th century, health education became increasingly sophisticated, incorporating new technologies and research into its approaches. Health education programs began to focus on specific populations, such as children, seniors, and people with special needs. In the 21st century, health education continues to evolve, focusing on the use of technology, the integration of health education into clinical settings, and the engagement of communities in health promotion.
Future Directions
As health education continues to evolve, it is likely to become even more sophisticated, incorporating new technologies and approaches. Health education programs may become more personalized, with an emphasis on individual needs and preferences. Technology may also be used to deliver health education, making it more accessible and engaging.
Analyzing How Technology is Changing Health Education
Technology is having a major impact on health education. Online learning platforms, social media, and virtual reality applications are being used to deliver health education in new and innovative ways. Let’s take a closer look at how technology is changing health education.
Online Learning Platforms
Online learning platforms, such as MOOCs (Massive Open Online Courses) and webinars, are being used to deliver health education. These platforms allow users to access health education materials from anywhere in the world, making it easier to reach a larger audience.
Use of Social Media
Social media is also being used to deliver health education. Platforms like Facebook and Twitter are being used to share health-related information, engage users in conversations, and encourage healthy behaviors.
Virtual Reality Applications
Virtual reality applications are being used to create immersive experiences that can be used to educate users about health-related topics. Virtual reality can be used to simulate medical procedures, allowing users to gain a better understanding of how the body works.

Investigating the Role of Health Education in Health Care Delivery
Health education is becoming increasingly important in health care delivery. It is being used to improve patient-provider communication, enhance self-care practices, and integrate health education into clinical settings. Let’s take a closer look at how health education is being used in health care delivery.
Integrating Health Education into Clinical Settings
Health education is being integrated into clinical settings to provide patients with information about their health conditions and treatments. Health care providers are using health education materials to explain diagnoses, provide instructions for self-care, and answer questions.
Enhancing Patient-Provider Communication
Health education can also be used to enhance patient-provider communication. By providing accurate information about health-related topics, health education can help patients understand their health conditions and treatments and make informed decisions about their care.
Supporting Self-Care Practices
Finally, health education can be used to support self-care practices. By providing information about healthy habits and behaviors, health education can help people make better decisions about their health and take steps to maintain their health.
Health education is a powerful tool for promoting health and wellness. It can be used to improve quality of life, increase awareness of health issues, and improve access to health care. It can also be used to reduce health disparities, inform policy development, and improve health outcomes. Furthermore, technology is changing the way health education is delivered, making it more accessible and engaging. Finally, health education is playing an increasingly important role in health care delivery, helping to improve patient-provider communication, enhance self-care practices, and integrate health education into clinical settings. In summary, health education is a valuable tool for promoting health and wellness.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
What Is Community Health and Why Is It Important?
By Ashley Brooks on 03/04/2019
- Share on Facebook
- Share on LinkedIn
- Share on Pinterest
- Share on Twitter

The community you live in is part of who you are. Even if you don’t see your neighbors every day, you recognize that the decisions you make impact those around you. You’re all in it together, and you wouldn’t have it any other way!
Improving your community and helping others is often at the top of your mind. So when the phrase “community health” crossed your radar, you had to know more. What is community health? And how does it affect the lives of those in your area?
Community health is the intersection of healthcare, economics and social interaction. Unfortunately, many people are unaware of the role this type of healthcare plays in their everyday lives. Join us as we explore the impact of community health on your neighborhood—and what you can do to improve it.
What is community health?
Community health is a medical specialty that focuses on the physical and mental well-being of the people in a specific geographic region. This important subsection of public health includes initiatives to help community members maintain and improve their health, prevent the spread of infectious diseases and prepare for natural disasters.
“Working at the community level promotes healthy living, helps prevent chronic diseases and brings the greatest health benefits to the greatest number of people in need,” reports the Centers for Disease Control and Prevention (CDC) . 1
Strong community health requires residents to look beyond themselves and take “collective responsibility,” says Caleb Backe, health and wellness expert at Maple Holistics . “It’s not just about the healthcare system, but focuses on the importance of leading a generally healthy lifestyle in order to protect the community as a whole.”
Community health is inextricably tied to individual wellness. “Good community health equates to healthy people, as a community is the ecosystem or environment in which people live,” says Thomas G. Bognanno, president and CEO of Community Health Charities . “It’s difficult to be healthy personally if your community is unhealthy.”
The far-reaching impact of community health
Community health flips the script on the old adage, “You take care of you; I’ll take care of me.” Instead, public health experts agree that the health of a community can have far-reaching—and sometimes surprising—impacts on individual health and beyond.
“Community health impacts everything—educational achievement, safety and crime, people’s ability to work and be financially healthy, life expectancy, happiness and more,” Bognanno says. “Health impacts every other facet of life, from a child’s ability to learn to an adult’s ability to work, so health is critical for education and financial well-being.”
The effect of health on quality of life can also impact the desire to participate in civic duties like voting, social functions and leisure activities, according to Healthy People 2020 , an initiative of the Office of Disease Prevention and Health Promotion. 2
Communities that are attentive to public health can even reduce inequality among their residents. “[Community health] also helps to reduce health gaps caused by differences in race and ethnicity, location, social status, income and other factors that can affect health,” reports the CDC . 1
The consequences of neglecting community health
A lack of focus on community health can lead to a range of complex problems that aren’t easy to correct. For example, crime and safety issues that result from neglected community health can quickly becoming a self-perpetuating cycle. “Repeated exposure to crime and violence may be linked to an increase in negative health outcomes. Children exposed to violence may show increased signs of aggression starting in upper-elementary school,” reports Healthy People 2020 . 2
Chronic diseases, such as diabetes and heart disease, can also increase if a community’s overall well-being is suffering. “An unhealthy community tends to be obese and struggle more from chronic diseases and other health challenges,” Bognanno says.
Chronic diseases like these not only reduce life expectancy, they have a dramatic effect on the economy. The CDC reports that 90 percent of the nation’s annual healthcare expenses are for people with chronic health conditions. 3
Curbing the spread of infectious disease is also a priority of community health programs. Without them, communities may find themselves battling outbreaks of illnesses that put vulnerable populations like the elderly at higher risk.
“If a community has to recover from an emergency event, such as a natural disaster, reducing the spread of disease becomes a crucial part of the recovery process,” Backe says.
Factors that improve community health
Improving community health is a huge undertaking that involves cooperation between public health workers, local government, volunteers and average citizens alike—and the end products of their work can take a lot of forms. “Communities benefit from walking trails and bike paths, from access to healthy food and playgrounds, from accessible healthcare services, schools and places of employment, as well as affordable housing,” Bognanno says.
Education also plays a large role in maintaining community health. Health fairs and advertising campaigns that expose the dangers of risk factors like tobacco exposure, poor nutrition and physical inactivity can raise awareness about the importance of choosing a healthy lifestyle. The CDC has also focused on promoting nutrition guidelines in schools and increasing the amount of physical education children receive. 4
Individuals can step up to the plate for their community’s health by volunteering at health fairs or blood drives, petitioning local officials to develop more green space and walking trails and maintaining their own health. “The collective responsibilities that individuals have for their communal health can lead to positive interactions within the community as a whole,” Backe says.
Take a stand for community health
What is community health? Now you know that it’s a vital component of public health—and it’s something every individual can play a part in improving. To learn more about how public health workers are improving the health of people across the nation, take a look at these articles, “ 6 Invaluable Ways Community Health Workers Improve Our Lives .” and " What Can You Do With a Health & Wellness Degree?"
Related Articles:
- 6 Examples of Positive Workplace Health Practices
- 11 Healthy Heart Tips to Help Keep the Doctor Away
- What's the Big Deal About Digital Health? Understanding This Revolution in Healthcare
1 Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Chronic Disease: A Significant Public Health Threat, [information accessed January 29, 2019] https://www.cdc.gov/nccdphp/dch/about/index.htm 2 Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services, Health-Related Quality of Life and Well-Being, [information accessed January 29, 2019] https://www.healthypeople.gov/2020/about/foundation-health-measures/Health-Related-Quality-of-Life-and-Well-Being 3 Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Health and Economic Costs of Chronic Diseases, [information accessed January 29, 2019] https://www.cdc.gov/chronicdisease/about/costs/index.htm 4 Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Partnerships to Improve Community Health, [information accessed January 29, 2019] https://www.cdc.gov/nccdphp/dch/programs/partnershipstoimprovecommunityhealth/index.html
Request More Information
Talk with an admissions advisor today.
Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid (for those who qualify)
- Customized Support Services
- Detailed Program Plans
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- No dashes, slashes or spaces
- No country code (e.g. "1" for USA)
- No numbers starting with "0" or "1"
There is an error in ZIP code. Make sure your answer has only 5 digits.
We offer tuition savings for many employers—see if yours is one of them.
Please enter Corporate Employer.
Can’t find your employer? Select "Other Employer Not In List" or "Not Employed".
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Ashley Brooks
Ashley is a freelance writer for Collegis education who writes student-focused articles on behalf of Rasmussen University. She believes in the power of words and knowledge and enjoys using both to encourage others on their learning journeys

Posted in Health and Wellness
Related Content

Hope Rothenberg | 10.17.2023

Carrie Mesrobian | 02.07.2022

Carrie Mesrobian | 01.31.2022

Ashley Brooks | 07.13.2020
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.
Health Education for Awareness and Behavioral Change and Influence
- Reference work entry
- First Online: 01 January 2019
- Cite this reference work entry

- Rita Campos 6 &
- Lúcia Fernandes 6
Part of the book series: Encyclopedia of the UN Sustainable Development Goals ((ENUNSDG))
314 Accesses
3 Citations
Ecosystem approach to health ; Education for sustainability ; Health literacy ; Health promotion ; Social mobilization
Health education comprises all experiences that can inspire changes in behavior leading to improved health and well-being and also improves health literacy, ultimately leading to a more conscious, empowered, and mobilized society (adapted from Nutbeam 2000 ). Health, as recognized by the World Health Organization, is “…a state of physical, mental and social well-being and not merely the absence of disease or infirmity” and well-being is a state of dynamic equilibrium between the physical, mental, and social challenges faced by people and their capacity to cope with it (adapted from Dodge et al. 2012 ).
Health Education, Health Literacy, and Empowerment
Health promotion and disease prevention have been common goals in health education programs. After almost six decades, health campaigns have moved the focus from the transmission of information based on...
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Adlong W, Dietsch E (2015) Environmental education and the health professions: framing climate change as a health issue. Environ Educ Res 21(5):687–709
Article Google Scholar
Allchin D (2009) The poisoning of Minamata. Minnesota: Universidade de Minnesota. [Online] Available at: douglasallchin.net/papers/MN-cases.pdf . Accessed 12 June 2018
Balvanera P, Siddique I, Dee L et al (2014) Linking biodiversity and ecosystem services: current uncertainties and the necessary next steps. Bioscience 64(1):49–57
Barbosa TMA (2010) A resposta a acidentes tecnológicos: o caso do acidente radioativo de Goiânia. Dissertação de Mestrado em Sociologia, Faculdade de Economia da Universidade de Coimbra
Google Scholar
Bernstein AS (2014) Biological diversity and human health. Annu Rev Public Health 35:153–167
Campbell-Lendrum D, Manga L, Bagayoko M et al (2015) Climate change and vector-borne diseases: what are the implications for public health research and policy? Philos Trans R Soc B 370:20130552
Campos R, Araújo M (2017) Traditional artistic expressions in science communication in a globalized world: contributions from an exploratory project developed in Northeast Brazil. Sci Commun 39(6):798–809
Campos R, Montenegro LA, Petrovich ACI et al. (In press) Práticas sustentáveis no cotidiano: divulgação do uso alternativo de materiais de limpeza. Anais do 8° Congresso Brasileiro de Extensão Universitária, Natal, 28–30 June. [Sustainable practices in daily life: divulgating alternative use of cleaning materials. Annals of the 8th Brazilian Congress of University Extension]
Campos R, Montenegro LA, Petrovich ACI et al. (submitted). Abordando a sustentabilidade, a economia doméstica e os problemas da água com produtos de limpeza. Actas do XIV Congresso da Sociedade Portuguesa de Ciências da Educação, Coimbra, Outubro 11–13. [Addressing sustainability, home economics and water problems with cleaning materials. Proceedings of the XIV Congress of the Portuguese Society of Educational Sciences]
Cardoso CW, Paploski IAD, Kikuti M et al (2015) Outbreak of exanthematous illness associated with zika, chikungunya, and dengue viruses, Salvador, Brazil. Emerg Infect Dis 21(12):2274–2276
Centemeri L (2008) Rispondere al disastro tecnologico. La lezione di Seveso. [Response to the technological disaster. Seveso's lesson.] Quaderno del Programma Emergenze di Massa, 8(1). Istituto di Sociologia Internazionale di Gorizia-ISIG, Gorizia
Chinn D (2011) Critical health literacy: a review and critical analysis. Soc Sci Med 73(1):60–67
Convention on Biological Diversity (1992) United Nations Conference on Environment and Development, Rio de Janeiro, 5–14 June. [Online]. Available at: http://www.cbd.int/convention/ . Accessed 12 June 2018
David B, Wolfender J-L, Dias DA (2015) The pharmaceutical industry and natural products: historical status and new trends. Phytochem Rev 14:299
Article CAS Google Scholar
Davis JM, Cooke SM (2007) Educating for a healthy, sustainable world: an argument for integrating health promoting schools and sustainable schools. Health Promot Int 22:346–353
Dodge R, Daly A, Huyton J, Sanders L (2012) The challenge of defining wellbeing. Int J Wellbeing 2:222–235
Edwards PJ, Abivardi C (1998) The value of biodiversity: where ecology and economy blend. Biol Conserv 83(3):239–246
Estacio EV (2013) Health literacy and community empowerment: it is more than just reading, writing and counting. J Health Psychol 18:1056–1068
European Social Survey (2015) Measuring and reporting on European’s wellbeing: findings from the European social survey. ESS ERIC, London
Ewing DA, Cobbold CA, Purse BV et al (2016) Modelling the effect of temperature on the seasonal population dynamics of temperate mosquitoes. J Theor Biol 400:65–79
Fernandes LO, Nunes JA, Porto MF (2016) Contaminação química: as respostas das instituições responsáveis e ações das populações atingidas no Brasil e em Portugal. [chemical contamination: the responses of the responsible institutions and actions of the affected populations in Brazil and Portugal.]. Saúde e Sociedade 25(1):218–232
Finn S, O’Fallon L (2017) The emergence of environmental health literacy – from its roots to its future potential. Environ Health Perspect 125:495–501
Forget G, Lebel J (2001) An ecosystem approach to human health. Int J Occup Med Environ Health 7(2):S3–S38
CAS Google Scholar
Fortun K (2001) Advocacy after Bhopal environmentalism, disaster, new global order. The University of Chicago Press, Chicago
Book Google Scholar
Freitas CM, Porto MFS, de Freitas NBB et al (2001) Chemical safety and governance in Brazil. J Hazard Mater 86:135–151
Gardner LM, Bóta A, Gangavarapu K et al (2018) Inferring the risk factors behind the geographical spread and transmission of Zika in the Americas. PLoS Negl Trop Dis 12(1):e0006194
Gonçalves ME (2007) Os portugueses e os novos riscos. [The Portuguese and the new risks.] Estudo e investigações, 45. Imprensa de Ciências Sociais, Lisboa
Gray KM (2018) From content knowledge to community change: a review of representations of environmental health literacy. Int J Environ Res Public Health 15(3):E466
Hancke D, Suárez OV (2014) Environmental health education in schools as strategy for rodent control: an experience in a shantytown of Buenos Aires, Argentina. EcoHealth 11:133–140
Harremoes P, Gee D, MacGarvin M et al. (2001) Late lessons from early warnings: the precautionary principle 1896–2000. Environmental report, European Environment Agency. Office for Official Publications of the European Communities, Copenhagen
Howard J (2006) Cover essay: children and EcoHealth. EcoHealth 3:215–217
Jennings V, Floyd MF, Shanahan D et al (2017) Emerging issues in urban ecology: implications for research, social justice, human health, and well-being. Popul Environ 39(1):69–86
Keniger LE, Gaston KJ, Irvine KN et al (2013) What are the benefits of interacting with nature? Int J Environ Res Public Health 10(3):913–935
Keune H, Kretsch C, De Blust G et al (2013) Science-policy challenges for biodiversity, public health and urbanization: examples from Belgium. Environ Res Lett 8(2):025015
Kim KH, Kabir E, Ara Jahan S (2014) A review of the consequences of global climate change on human health. J Environ Sci Health 32:299–318
McCallum ML (2015) Vertebrate biodiversity losses point to a sixth mass extinction. Biodivers Conserv 24(10):2497–2519
Millennium Ecosystem Assessment (2005) Ecosystems and human well-being: synthesis. Island Press, Washington
Morrison AC, Zielinski-Gutierrez E, Scott TW et al (2008) Defining challenges and proposing solutions for control of the virus vector Aedes aegypti. PLoS Med 5(3):e68
National Research Council (2011) Climate stabilization targets: emissions, concentrations, and impacts over decades to millennia. The National Academies Press, Washington
Nunes JA, Matias M (2006) Rumo a uma saúde sustentável: saúde, ambiente e política. Saúde e Direitos Humanos 3:7–15
Nutbeam D (2000) Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 15(3):259–267
Petryna A (2002) Life exposed: biological citizens after Chernobyl. Princeton University Press, Princeton
Pimm SL, Jenkins CN, Abell R et al (2014) The biodiversity of species and their rates of extinction and protection. Science 344:987–997
Pradhan P, Costa L, Rybski D, Lucht W, Kropp JP (2017) A systematic study of sustainable development goal (SDG) interactions. Earth’s Future 5:1169–1179
Romanelli C, Corvalan C, Cooper HD, Manga L, Maiero M, Campbell-Lendrum D (2014) From Manaus to Maputo: toward a public health and biodiversity framework. EcoHealth 11(3):292–299
Sala OE, Meyerson LA, Parmesan C (2012) Biodiversity change and human health: from ecosystem services to spread of disease. Island Press, Washington
Sørensen K, Van den Broucke S, Fullam J et al (2012) Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 12:80
Stone-Jovicich S, Goldstein BE, Brown K et al (2018) Expanding the contribution of the social sciences to social-ecological resilience research. Ecol Soc 23(1):41–48
ten Brink P, Mutafoglu K, Schweitzer J-P et al (2016) The health and social benefits of nature and biodiversity protection. Background report for a workshop by the European Commission (ENV.B.3/ETU/2014/0039). Institute for European Environmental Policy, London/Brussels
Wallerstein N, Bernstein E (1988) Empowerment education: Freire’s ideas adapted to health education. Health Educ Q 15:379–394
WHO – World Health Organization (2016) WHO situation report: Zika Virus, microcephaly and Guillain-Barre syndrome. WHO, World Health Organization [Online] Available at: http://apps.who.int/iris/handle/10665/250724 . Accessed 02 July 2018
WHO – World Health Organization (2017) Media Center: Vector-borne diseases. [Online] Available at: http://www.who.int/mediacentre/factsheets/fs387/en/ . Accessed 12 June 2018
WHO – World Health Organization, UN Environment Programme, Convention on Biological Diversity (2015) Connecting global priorities: biodiversity and human health: a state of knowledge review. [Online] Available at: http://www.cbd.int/en/health/stateofknowledge . Accessed 12 June 2018
Wilcox B, Kueffer C (2008) Transdisciplinarity in ecoHealth: status and future prospects. EcoHealth 5(1):1–3
Zanluca C, Melo VCA, Mosimann ALP et al (2015) First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz 110(4):569–572
Download references
Acknowledgments
RC and LF are supported by Fundação para a Ciência e a Tecnologia (FCT, Portugal): grants SFRH/BPD/110348/2015 and SFRH/BPD/79933/2011 (POCH funds from ESF and MCTES), respectively, and Contrato-Programa to RC (NT of the DL 57/2016 altered by Law 57/2017). The Biodiversity Workshops were developed within the framework of the program “CES vai à Escola” (“CES goes to School”; https://www.ces.uc.pt/extensao/cesvaiaescola/?id_lingua=2 ), funded by CES-UC via FCT (UID/SOC/50012/2013).
Author information
Authors and affiliations.
CES-UC – Centre for Social Studies, University of Coimbra, Coimbra, Portugal
Rita Campos & Lúcia Fernandes
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rita Campos .
Editor information
Editors and affiliations.
European School of Sustainability Science and Research, Hamburg University of Applied Sciences, Hamburg, Germany
Walter Leal Filho
International Centre for Thriving, University of Chester, Chester, UK
Center for Neuroscience and Cell Biology and Institute for Interdisciplinary, Research of the University of Coimbra, Coimbra, Portugal
Anabela Marisa Azul
Passo Fundo University Faculty of Engineering and Architecture, Passo Fundo, Brazil
Luciana Brandli
Istinye University, Istanbul, Turkey
Pinar Gökcin Özuyar
Section Editor information
No affiliation provided
Mohamed Walid
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry.
Campos, R., Fernandes, L. (2020). Health Education for Awareness and Behavioral Change and Influence. In: Leal Filho, W., Wall, T., Azul, A.M., Brandli, L., Özuyar, P.G. (eds) Good Health and Well-Being. Encyclopedia of the UN Sustainable Development Goals. Springer, Cham. https://doi.org/10.1007/978-3-319-95681-7_99
Download citation
DOI : https://doi.org/10.1007/978-3-319-95681-7_99
Published : 26 September 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-95680-0
Online ISBN : 978-3-319-95681-7
eBook Packages : Earth and Environmental Science Reference Module Physical and Materials Science Reference Module Earth and Environmental Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
Community health education is an important part of our world today. In fact, if the year 2020 has taught us anything, it is that community health education is a vital part of our society. The outbreak of COVID-19 - a pandemic that has infected millions of people around the world — crippled the global economy and changed the way we live. ...
Education is a process and a product.From a societal perspective, the process of education (from the Latin, ducere, "to lead," and e, "out from," yield education, "a leading out") intentionally engages the receptive capacities of children and others to imbue them with knowledge, skills of reasoning, values, socio-emotional awareness and control, and social interaction, so they can ...
Importance of Health Education - Health education is important for individuals, families, and communities. It can help people learn about their health, make healthy choices, and reduce their risk of disease. Health education plays a crucial role in improving individual and community well-being.
Why Community Health Is Important. ... An education or early career in community health sciences can form a solid foundation for a career in medicine as a physician, psychiatrist, or nurse practitioner, and might even lead the health professional to practice in an at-risk geographic area. A community health worker might also go on to become a ...
The importance of health education also extends into policy and legislation development at a local, state and national level, informing and influencing key decisions that impact community health. From campaigns and legislation to enforce seat belt use and prevent smoking to programs that boost the awareness and prevention of diabetes, public ...
Social and community context, another important social determinant of health, encompasses: Civic activities - voting, volunteering, and participating in community groups ... Public health professionals play a key role in program coordination, health advocacy and education, management, and community health services. Careers in public health ...
Health education is an important component of the public health system. It involves the dissemination of information and skills that enable individuals to make informed decisions about their health. ... By providing health education programs, community organizations can help people become more aware of health issues, learn healthy habits and ...
Rasmussen University is accredited by the Higher Learning Commission and is authorized to operate as a postsecondary educational institution by the Illinois Board of Higher Education. For additional information about Licensing and State Authorization, and State Contact Information for Student Complaints, please see those sections of our catalog .
How health education programs can help target populations learn about specific health topics, as a strategy for health promotion and disease prevention. ... Importance of Sustainability; ... Examples of health education interventions in community paramedicine are available in the Rural Community Paramedicine Toolkit. Health education is also ...
Health education comprises all experiences that can inspire changes in behavior leading to improved health and well-being and also improves health literacy, ultimately leading to a more conscious, empowered, and mobilized society (adapted from Nutbeam 2000).Health, as recognized by the World Health Organization, is "…a state of physical, mental and social well-being and not merely the ...